Sustainable Healthcare Plastics: Rethinking Design, Use, and Recovery

Plastics save lives, and the next frontier in medical innovation is making them as sustainable as they are essential.
Plastics have become essential over the decades, evolving into the backbone of modern healthcare. Polymer-based materials enable life-saving interventions every day, from sterile barriers and flexible catheters to lightweight components for imaging systems and single-use surgical instruments. But the same attributes that make plastics indispensable—sterility, low weight, and low cost—also contribute to one of the most complex and voluminous waste streams in the sector.
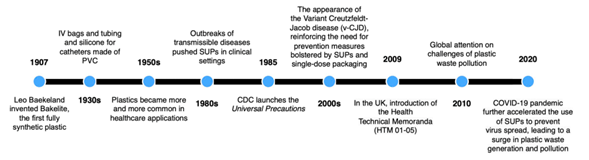
Timeline of plastics in healthcare and relevant regulations/events that spurred its use. Courtesy of Advancing the circular economy of healthcare plastics: A systematic literature review.
A recent systematic review published in Resources, Conservation & Recycling sharply focuses on this issue. The authors compiled and analyzed 242 studies, mapping worldwide plastic use across healthcare systems. The conclusion is clear: while recycling initiatives are expanding, they are not sufficient. True circularity in healthcare plastics must begin at the design stage and carry through the entire product life cycle.
You can also read: How to Transform Healthcare Plastics Circularity
Understanding the Scale of Healthcare Plastic Waste
The study offers rare quantitative insights into waste generation. Hospitals, for example, generate an average of 0.44 kilograms of plastic waste per patient daily. Individual medical procedures typically yield between 0.4 and 3 kilograms of plastic, although in some Danish surgical departments the figure can climb to 16 kilograms per procedure. At the national level, the volume is staggering. The United States alone produces an estimated 1.7 million metric tons of healthcare plastic waste annually, followed by Germany at 125,000 metric tons and Saudi Arabia at 15,000.
Even though the World Health Organization estimates that 85 percent of medical waste is non-hazardous, hospitals still incinerate or landfill most of it. Systemic misclassification drives this problem. Staff often treat uncontaminated items as infectious out of caution or habit. The authors call this practice “hygienic obsolescence,” which blocks any chance of reuse or recycling. The impact reaches beyond hospitals: in 2024, medical debris surged onto U.S. beaches, forced closures, and exposed the environmental risks of current waste handling methods.
Circular Strategies: The 8Rs in Practice
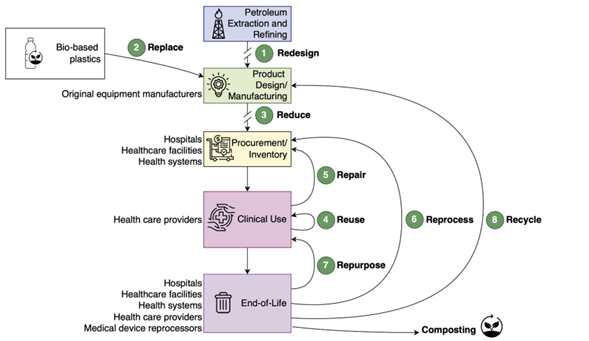
Circular economy strategies for healthcare plastics, including life cycle stages and main stakeholders responsible for each. Courtesy of Advancing the circular economy of healthcare plastics: A systematic literature review.
To address this growing problem, the authors propose a framework built on eight circular strategies: redesign, replace, reduce, reuse, repair, reprocess, repurpose, and recycle. Among these, redesign and reuse have seen the most research activity and implementation momentum since 2020. Reprocessing of single-use devices (SUDs) is also gaining regulatory acceptance, although the topic of repair remains surprisingly underexplored, despite its relevance for long-life equipment. Recycling, while the most familiar approach, is the least effective when used in isolation and without upstream design interventions.
Technical Pathways Toward Circularity
Redesign is a critical starting point. It means rethinking polymer selection, component architecture, and packaging formats with the end of life in mind. The review highlights several engineering strategies. One is to simplify material mixes so recyclers can separate them more easily. Another is to choose polymers that are chemically compatible when products combine different materials. A third is to develop designs that tolerate repeated sterilization. For example, switching from multilayer barrier films to mono-material packaging, such as thinner syringe wrap films, can keep products sterile and allow recycling. Additive manufacturing technologies like 3D printing also help. When manufacturers power these systems with recycled thermoplastics, they cut waste during production and gain the advantage of custom designs.
Material Innovation and Substitution
Material replacement is also gaining traction. Researchers are testing bio-based and biodegradable polymers such as PLA, PHA, PCL, and P3HB-4HB for applications with lower mechanical or chemical demands. Other advances include phthalate-free plasticizers for PVC and fiber-based materials for diagnostic casings. Companies now phase out expanded polystyrene foam, often used in cold-chain logistics, and switch to materials like ClimaCell, which cut emissions by 65 percent. However, the review urges decision-makers to use life cycle assessment when they choose new materials to avoid unintended consequences.
Operational Shifts and Reuse Strategies
Operational changes also present opportunities to reduce plastic consumption. Hospitals have introduced checklists that minimize the number of instruments opened pre-surgery, reducing waste from unused disposables. Waste segregation protocols that separate clean, non-infectious plastics from hazardous materials allow for targeted recycling or reuse. Denmark’s Region Zealand, for instance, has piloted successful interventions in surgical departments, showing that frontline clinical practices can make a measurable impact.
The reuse and reprocessing of devices, long considered off-limits, are becoming technically and legally viable again. Third-party reprocessors regulated by the FDA are handling SUDs such as catheters, laparoscopic tools, and electrophysiology devices. Hospitals are also reintroducing reusable gowns, face masks, and scrub caps. Sterilization methods like low-temperature vaporized hydrogen peroxide and ultraviolet germicidal light (UVGI) ensure that reused equipment meets safety standards. Studies show that reusable PPE can reduce waste by over 60 percent while offering comparable or better protection than disposables.
In cases where recycling does not work, repurposing offers a path forward. The review cites examples in which teams disinfect syringes and PPE, shred them, and then mix the fragments into asphalt or concrete to reinforce road construction. These applications, still experimental, show how high-volume, low-grade plastics can stay in the economy.
Recycling remains essential, especially for clean, mono-material waste streams. Mechanical recycling works for items like IV bags and syringe casings. Researchers are developing chemical recycling methods, including pyrolysis and catalytic hydrocracking, for more complex or contaminated plastics. These processes show promise in recovering high-quality monomers from mixed polyolefin waste but need further testing to validate environmental performance and cost-effectiveness.
Structural Barriers Remain
Despite the growing toolkit, the study identifies five key barriers to widespread adoption of circular strategies. First, inconsistent classification and sorting systems make it difficult to capture recoverable materials. Second, complex product design, especially the use of incompatible or unrecyclable polymers, prevents material recovery. Third, hospital workloads stretch staff and leave them without time or training in sustainable waste practices. Fourth, regulatory frameworks still emphasize single-use models in the name of infection prevention, which discourages innovation. Finally, weak market demand for recycled or bio-based plastics, combined with higher costs, limits their deployment.
A Path for Industry Leadership
The authors conclude that transforming healthcare plastics into a circular system is both a technical and institutional challenge. It will require coordination between product designers, materials scientists, hospital procurement teams, and regulators. Design-for-recovery must become standard practice. Economic incentives, such as extended producer responsibility, recycling targets, and green procurement criteria, could encourage circular business models.
For polymer producers and medical device manufacturers, this transition presents an opening. Hospitals are facing increasing pressure to meet environmental goals. Suppliers who offer validated, safe, and cost-effective solutions that enable material recovery and reuse will become valuable partners in a new generation of sustainable healthcare.
Read the full article here: Advancing the circular economy of healthcare plastics: A systematic literature review
